Global Health at Risk: Addressing Antimicrobial Resistance in Asia, Africa, and the Middle East
Global Health at Risk: Addressing Antimicrobial Resistance in Asia, Africa, and the Middle East
A silent pandemic: the rising tide of antimicrobial resistance
Antimicrobial resistance (AMR) is a critical global health threat that undermines the effectiveness of antibiotics, leading to increased mortality, prolonged illnesses, and higher healthcare costs. According to the World Health Organization (WHO) 2024 report, AMR is responsible for at least 1.27 million deaths annually and is associated with nearly 5 million deaths globally. Addressing AMR is crucial for global health security, as it threatens to reverse decades of medical progress, compromise the treatment of infectious diseases, and hinder the achievement of sustainable development goals. The rise of AMR means that common infections and minor injuries, which have been treatable for decades, can once again become deadly. This situation is exacerbated by the overuse and misuse of antibiotics in humans, animals, and agriculture, which accelerates the development of resistant bacteria. The health impact includes increased mortality, prolonged illnesses, and higher healthcare costs due to more complex and prolonged treatments.
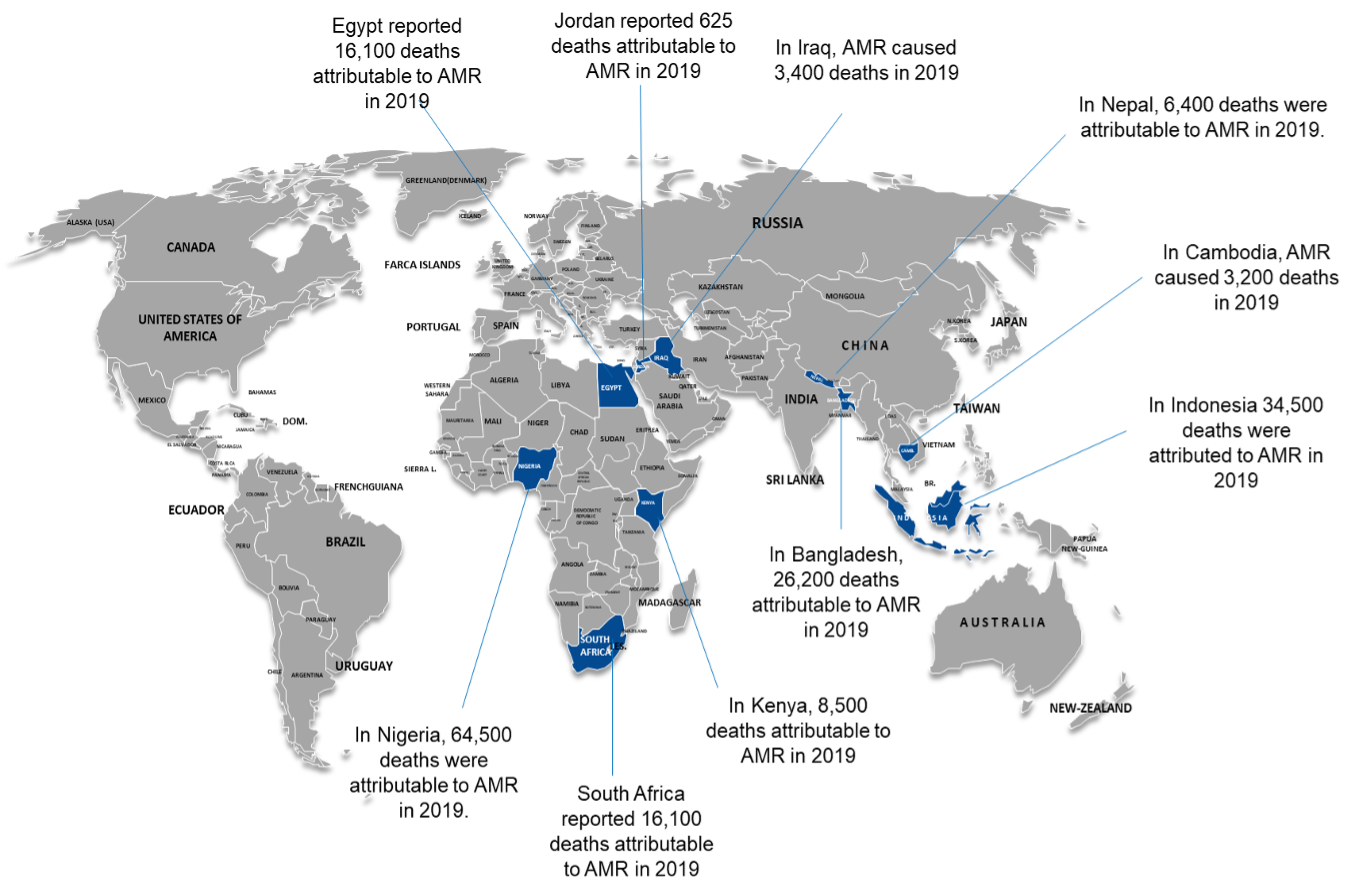
Economically, AMR could cause a loss of up to $100 trillion in global economic output by 2050, affecting livelihoods and productivity, especially in low- and middle-income countries. Developmentally, AMR undermines efforts to achieve several Sustainable Development Goals (SDGs), including those related to health, poverty, and economic growth, and threatens food security due to the use of antibiotics in agriculture. In this commentary, we reviewed the AMR burden in 10 countries in Africa, Asia, and the Middle East, highlighting the critical roles of governments, research institutions, universities, pharmaceutical companies, donors, and other stakeholders in addressing this public health crisis. See map- developed by AGI.
AMR in selected countries
Asia’s battlefront: Confronting AMR in Bangladesh, Nepal, Cambodia, and Indonesia
- Bangladesh faces a high burden of AMR, with 26,200 deaths attributable to AMR in 2019. The country has implemented a National Action Plan (NAP) focusing on surveillance, infection prevention, and antimicrobial stewardship. However, challenges remain in ensuring consistent data collection and improving laboratory capacities. Strengthening public awareness and integrating AMR strategies across human, animal, and environmental health sectors are crucial steps forward.
- Nepal‘s AMR situation is alarming, with 6,400 deaths attributable to AMR in 2019. The National Action Plan (2021-2026) emphasizes a One Health approach, aiming to improve surveillance, optimize antimicrobial use, and enhance infection prevention. Key challenges include the irrational use of antimicrobials and inadequate healthcare infrastructure. Enhancing intersectoral coordination and investing in modern diagnostic tools are essential for effective AMR containment.
- In Cambodia, AMR caused 3,200 deaths in 2019. The country has a Multi-Sectoral Action Plan (2019-2023) focusing on surveillance, infection control, and antimicrobial stewardship. Despite these efforts, gaps in laboratory capacity and data management persist. Strengthening laboratory networks and ensuring sustainable financing for AMR activities are critical for progress.
- Indonesia reported 34,500 deaths attributable to AMR in 2019. The National Strategy for Controlling AMR (2025-2029) aims to enhance governance, improve surveillance, and promote rational antimicrobial use. Challenges include high antimicrobial consumption and limited access to quality healthcare. Implementing robust surveillance systems and promoting public awareness campaigns are vital for mitigating AMR.
Africa’s challenge: tackling AMR in Kenya, South Africa, and Nigeria
- Kenya faces a significant AMR burden, with 8,500 deaths attributable to AMR in 2019. The National Action Plan emphasizes a One Health approach, integrating human, animal, and environmental health. Key challenges include inadequate laboratory infrastructure and limited public awareness. Strengthening laboratory capacities and enhancing community engagement are essential for effective AMR control.
- South Africa reported 16,100 deaths attributable to AMR in 2019. The National Strategy Framework (2018-2024) focuses on surveillance, antimicrobial stewardship, and infection prevention. Despite progress, challenges remain in ensuring consistent data collection and addressing disparities in healthcare access. Investing in laboratory infrastructure and promoting equitable healthcare access are crucial for combating AMR.
- Nigeria has one of the highest AMR burdens, with 64,500 deaths attributable to AMR in 2019. The Second National Action Plan (2024-2028) aims to enhance surveillance, improve antimicrobial stewardship, and strengthen healthcare systems. Key challenges include weak healthcare infrastructure and limited funding. Ensuring sustainable financing and improving healthcare infrastructure are vital for effective AMR containment.
Middle Eastern frontlines: addressing AMR in Jordan, Iraq, and Egypt
- Jordan reported 625 deaths attributable to AMR in 2019. The National AMR Surveillance System, established in 2017, focuses on improving laboratory capacities and enhancing surveillance. Challenges include limited public awareness and inadequate infection control practices. Strengthening public awareness campaigns and investing in infection control measures are essential for progress.
- In Iraq, AMR caused 3,400 deaths in 2019. The country faces significant challenges in implementing effective AMR strategies due to ongoing conflicts and limited healthcare infrastructure. Enhancing healthcare infrastructure and promoting international collaborations are crucial for addressing AMR.
- Egypt reported 16,100 deaths attributable to AMR in 2019. The National Action Plan (2018-2022) focuses on surveillance, antimicrobial stewardship, and infection prevention. Despite these efforts, challenges remain in ensuring consistent data collection and addressing healthcare disparities. Strengthening laboratory networks and promoting equitable healthcare access are essential for combating AMR.
United against AMR: the role of stakeholders in addressing AMR
- Governments are responsible for implementing national action plans, regulating antimicrobial use, and ensuring the availability of quality healthcare services. They must allocate sufficient resources to AMR initiatives and foster intersectoral collaboration to address the issue comprehensively.
- Research Institutions and Universities contribute to understanding AMR mechanisms, developing new diagnostic tools, and evaluating the effectiveness of interventions. They should collaborate with other stakeholders to translate research findings into practical solutions.
- Pharmaceutical Companies play a crucial role in developing new antibiotics and alternative therapies. They must invest in research and development to bring new antimicrobial agents to market and ensure responsible marketing practices to prevent the overuse and misuse of antibiotics.
- Donors and International Organizations provide essential funding and technical support for AMR initiatives. They must ensure that resources are used effectively and support capacity-building efforts in low- and middle-income countries.
- Healthcare Providers are on the front lines of combating AMR. They must adhere to best practices in prescribing antibiotics, implement infection control measures, and educate patients about the importance of responsible antimicrobial use.
- Public and Private Sector Collaboration between the public and private sectors is vital for addressing AMR. Joint efforts can enhance surveillance, improve access to diagnostics and treatments, and promote public awareness campaigns.
A call to action: strengthening global efforts to combat AMR
Effectively addressing AMR necessitates a coordinated, multi-sectoral approach that integrates human, animal, and environmental health. Key strategies include strengthening laboratory capacities, promoting responsible antimicrobial use, enhancing surveillance systems, ensuring sustainable financing, and fostering international collaboration. These efforts are vital for countries to make substantial progress in combating AMR and protecting public health.
References
- CDC Antimicrobial Resistance Facts and Stats
- WHO AMR Resource Pack 2024
- Health Data on AMR in Bangladesh
- National AMR Web Portal – AMR
- AMR Bangladesh Dashboard
- Health Data on AMR in Nepal
- Nepal National Action Plan for AMR
- Nepal AMR National Action Plan
- Health Data on AMR in Cambodia
- Cambodia AMR Multi-Sectoral Action Plan
- Cambodia AMR Country Profile
- Health Data on AMR in Indonesia
- WHO Indonesia AMR Strategy
- WHO Monitoring AMR in Indonesia
- Health Data on AMR in Kenya
- Kenya AMR NAP M&E Framework
- Kenya National Action Plan on AMR
- Health Data on AMR in South Africa


